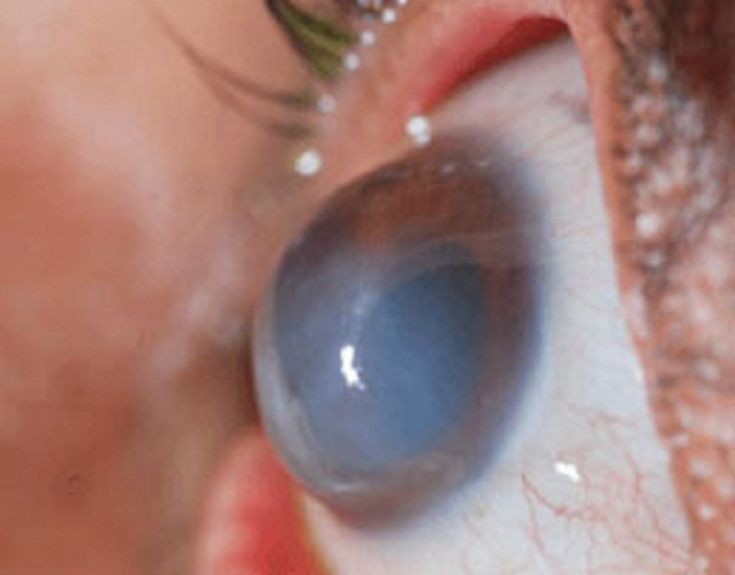
Keratoconus

What Happens in Keratoconus?
Keratoconus is an eye condition where the normally round, dome-shaped cornea gradually becomes thin and bulges outward into a cone-like shape. This irregular shape prevents light from focusing properly on the retina, leading to blurred, distorted, or ghosted vision.
It often begins in the teenage years or early adulthood and may progress slowly over time. As the cornea becomes more conical, patients may experience increased sensitivity to light, frequent changes in their glasses prescription, and difficulty seeing clearly, especially at night.
In advanced stages, glasses alone may not provide clear vision, and patients might need specialized contact lenses or surgical options to manage the condition. Early detection and regular monitoring are crucial to slow down progression and preserve vision.
Why Does Keratoconus Happen?
Keratoconus develops when the cornea (the clear front part of the eye) becomes weaker and thinner over time, losing its regular shape. Instead of staying round, it starts bulging outward like a cone.
When Does Keratoconus Begin?
It may start in childhood or teenage years, but often goes unnoticed until blurred vision prompts an eye check-up. It can progress quickly during adolescence and is often linked to chronic eye rubbing or severe eye allergies.
How is Keratoconus Diagnosed?
Mild cases of keratoconus can often go unnoticed during a routine eye check-up, especially in the early stages when symptoms are subtle. For a precise and reliable diagnosis, we use Corneal Topography (Pentacam)—a specialized imaging tool that creates a highly detailed 3D map of the cornea. This advanced scan detects even the slightest changes in the cornea’s shape, thickness, and curvature, allowing us to identify keratoconus at its earliest stage, even before noticeable vision problems arise.

Can Keratoconus Be Cured?
There is no permanent cure for keratoconus, but the condition can be managed effectively with timely treatment to preserve and improve vision. Early diagnosis and intervention are key to preventing further damage. Various options like specialized contact lenses, collagen cross-linking, or surgical procedures can help depending on the severity. Regular follow-ups with an eye specialist are essential to monitor changes and adjust the treatment plan as needed for the best visual outcomes.
Keratoconus Treatment Includes Two Key Steps
- Stabilizing the condition
- Improving vision
Stabilization (C3R)
We use an advanced technique called Corneal Collagen Cross-Linking (C3R) with Riboflavin to halt the progression of keratoconus. This procedure is designed to strengthen the weakened cornea and prevent further bulging.
During the procedure, the outermost layer (epithelium) of the cornea is gently removed to allow better penetration of riboflavin (Vitamin B2) eye drops into the corneal tissue. Once the riboflavin is adequately absorbed, the cornea is exposed to ultraviolet A (UVA) light at a controlled wavelength. This interaction between riboflavin and UV light triggers a chemical reaction that creates new collagen bonds within the corneal structure, increasing its strength and stability.
Important
This treatment is not meant to improve vision directly. Its primary goal is to prevent further deterioration of the cornea and stop the progression of the disease.
Vision Improvement Options
Each eye is different, so treatment is tailored individually. Here are the main options
- 1. Spectacles: Suitable for mild keratoconus with low power and good vision.
- 2. Special Contact Lenses: For moderate cases where glasses are not effective. These include rigid gas-permeable, scleral, or hybrid lenses.
- 3. Intracorneal Rings (ICRs): Small plastic inserts placed inside the cornea to reduce its steepness and improve its shape.
- 4. Phakic Intraocular Lenses (ICLs): For patients with very high prescriptions not correctable by rings or lenses.
- 5. Corneal Transplant: Considered when the cornea is very thin or scarred. Options include full-thickness or partial-thickness grafts depending on severity.
Can LASIK Be Done in Keratoconus?
No, LASIK is not recommended for patients with keratoconus. In fact, it is considered an absolute contraindication.
Keratoconus is a condition where the cornea becomes thin and bulges outward, resulting in a cone-like shape. LASIK involves removing corneal tissue to reshape the surface and correct vision. Performing LASIK on an already weakened and thinned cornea—as seen in keratoconus—can further destabilize the eye and worsen the condition, potentially leading to severe visual impairment or even corneal damage that may require a transplant.
Why LASIK Is Unsafe in Keratoconus
- Thinner corneas cannot safely tolerate the removal of tissue required in LASIK.
- It may lead to corneal ectasia, a serious condition where the cornea becomes even more unstable after surgery.
- It can cause rapid deterioration of vision rather than improvement.